In an article in the New York Times today, My Medical Choice, Angelina Jolie promised to share some background about her medical treatment with women seeking more information about BRCA gene mutations and what it might mean for them. This blog describes the main stages of her treatment.
It is important to emphasize that each woman’s case is different. Surgery will not necessarily be the right choice for everyone, and there are alternatives available. As Angelina says in her article, the important thing is to be aware of your options.
 We’ve been working hard on this. Add your e-mail address and we will tell you as soon as it launches.
We’ve been working hard on this. Add your e-mail address and we will tell you as soon as it launches.
Stage 1. Gathering Data and Information
- BRCA stands for BReast CAncer. BRCA genes help you fight cancer when it happens in your body. But some families carry mutated or broken BRCA genes that can be passed down from one generation to the next. Approximately 5-10% of all breast cancers and 14% of ovarian cancers occur from a BRCA1 or BRCA2 genetic mutation that is inherited from either parent.
- Women carrying BRCA1 or BRCA2 gene mutations have up to an 87% lifetime chance of breast cancer and 54% chance of ovarian cancer vs. a general population risk of 12% for breast cancer and less than 1% for ovarian cancer. Prevention does not yet exist. More details about the risks of breast and ovarian cancer, including how risk changes with each decade of life, can be found in our BRCA Gene Mutations blog post.
- Given the high likelihood of getting breast or ovarian cancer with BRCA mutations, family history usually triggers testing for the gene. Angelina’s mother had breast cancer, and sadly passed away from ovarian cancer. Her maternal grandmother was also diagnosed with ovarian cancer. This family history would certainly meet any insurance carrier’s criteria to cover genetic testing. To find out if there is enough risk for you to consider a BRCA mutation genetic test, we encourage you to take our Genetics Quiz that reviews a variety of information, including your family history.
Get discounted Tier 2 tickets while they last. Watch the Summit via on-demand video from anywhere or attend in person at the breathtaking oceanfront Terranea Resort in Southern California.
Stage 2. After diagnosis: Traveling the Road of Surveillance
We follow a standard surveillance plan at our center for BRCA mutation carriers, which I used for Angelina:
Beginning at age 18, or 10 years younger than the youngest relative with breast cancer, every 3 months, you have breast imaging or an exam. An example plan follows:
- Month 1:
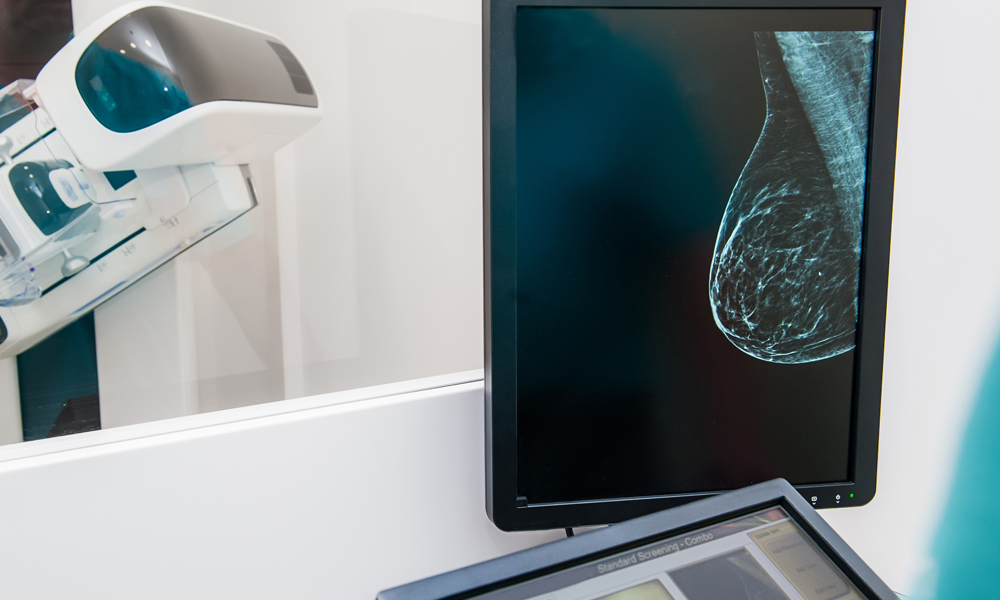
Mammogram (wait until 25 years old)
Whole breast screening ultrasound (begin at 18)
- Month 4:
Clinical breast exam with a breast specialist
- Month 7:
Breast MRI, timed to menstrual cycle days 7-10 (day 1 is the day bleeding starts); Contrast Enhanced Spectral Mammography (CESM) for those who cannot have an MRI
- Month 10:
Clinical breast exam with a breast specialist
- Every month:
Self breast exams (cycle days 7-10). If you don’t know how to do a self breast exam, please watch our how-to video.
For those who prefer twice-a-year surveillance, we combine the imaging with clinical breast exams, and meet every 6 months.
Ovarian surveillance begins at age 35, or 10 years prior to youngest relative with ovarian cancer, and includes the following:
- Transvaginal Pelvic ultrasound every 6 months (cycle days 1-10)
- CA-125 blood marker testing every 6 months (after cycle day 5)
- Pelvic exam by gynecologist every 6 months
For additional screening details, including risk reduction strategies and holistic and integrative medicine, see our blog on BRCA Gene Mutations.
Follow Power Up
Follow Power Up
Stage 3. Committing to an operation
When first meeting a woman newly diagnosed with a BRCA mutation, my immediate goal is to learn about her, including her family situation, whether she is in a stable relationship, and whether she is planning to have children. In the course of these discussions, it becomes clear whether the patient will proceed to a mastectomy.
Stage 4. Preparing for the operations
The questions any patient needs to address at this stage include: (1) whether or not to preserve the nipples, (2) if so, whether or not to perform a “nipple delay” procedure, (3) where to place the incision, (4) whether or not to test sentinel nodes, (5) what kind of reconstruction will be done, (6) what supplements might enhance healing and recovery, and finally (7) where should we operate.
NIPPLE: Women undergoing preventive mastectomies can always consider keeping their nipples. While no one can guarantee that the nipples will survive an operation, much can be done to ensure the greatest chance of success.
NIPPLE DELAY: The delay, performed 1-2 weeks prior to the actual mastectomies, uses the planned mastectomy incision and lifts half of the skin off of the breast surface. A small disc of the tissue directly behind the nipple and areola is also removed and analyzed by a pathologist. This is done to rule out the presence of any disease directly behind the nipples, which would make preserving them a dangerous proposition. Additionally, it recruits extra blood flow to the area, lessening the chances of nipple and skin loss due to insufficient blood supply after the mastectomy. Since starting this technique in 2008, my loss of skin and nipple after mastectomy has decreased to less than 2%. In Angelina’s case, she judged it worth taking this extra step of caution.
INCISION: Incision locations must take into consideration a cancer location (if cancer is present), any prior incisions, breast size reduction (if desired), and the technical skill of the surgeon (smaller incisions make for a harder and longer operation). For Angelina, her optimal incision choices were around the areola, or underneath the breast in the inframammary fold – the latter was chosen.
SENTINEL NODE BIOPSY/PBDI: Whenever a breast contains cancer and the armpit lymph nodes cannot be felt on exam, we routinely perform a sentinel node biopsy, which is the removal of the first nodes that receive breast lymphatic drainage. By injecting blue dye into the breast, which then travels to the lymph node(s), we find out if cancer spread beyond the breast. Until now, the trend has been not to perform sentinel node biopsies in conjunction with prophylactic (preventive) mastectomies since the discovery of cancer in breasts removed prophylactically only ranges from 2-8%. Therefore, most women do not want to take the additional risks associated with a sentinel node biopsy, especially since they can have complications, such as pain, numbness, arm swelling (lymphedema), fluid buildup (seroma), limited arm movement, and infection. This dilemma has been resolved with a new technique that was pioneered at the Pink Lotus Breast Center, called Prophylactic Breast Dye Injection, or PBDI. PBDI allows the sentinel node to be identified, but not surgically removed, giving more control and peace of mind to women. I developed this technique while treating Angelina, and I hope other women will now benefit from it. It was at her friendly insistence that I wrote the rationale for it in our blog post, Prophylactic Breast Dye Injection.
RECONSTRUCTION: Reconstruction options vary depending on a number of factors. The two broad categories of reconstruction include implants and flaps. Implants are the most common reconstruction, often requiring two stages, whereby a tissue expander is placed prior to the final implant. A tissue expander is a deflated implant that goes behind the pectoral muscles and gets slowly inflated with saline over a period of 2-3 months, until the chosen volume is reached. A second operation is performed to swap the expander for the final implant (usually silicone). A different implant option can be a “one-step” operation, where the final implant is placed at the time of mastectomy, skipping the expander phase.
Two improvements which I believe can enhance the final outcome for those patients choosing implants include: (1) the newly FDA-approved anatomic implants, which are teardrop shaped, and (2) allograft, or synthetic sheets of material, that create a more natural look.
Autologous flaps use your own skin, fat and sometimes muscle from the abdomen, back (latissimus), thigh (gracilis), or buttock to create a potentially more natural breast reconstruction than implants can achieve. Flaps, however, create scars at the donor site, potential weakness in the donor area, and involve a longer operation than implants, with longer recovery periods and associated hospital stays.
Angelina’s body type was best suited to an implant reconstruction with allograft. Although tissue expanders required an additional operation, she preferred to use them. Expanders maximize blood flow to the breast skin and nipple (because they are not fully expanded right after placement, they do not compress the tiny blood vessels in the skin), and they allow us to optimize the final implant size, location and appearance.
SUPPLEMENTS AND PREP: To prepare for and to recover from operations, patients can use a variety of supplements. Angelina followed the regimen below, written onto a calendar:
To enhance wound healing (for each operation):
A) Vitamin C: 1000mg tablets; one tablet once daily for one week before and one week after surgery.
B) Multi-Vitamin: one tablet once daily for one week before and one week after surgery.
C) Zinc: 50 mg; one tablet once daily for one week before and one week after surgery.
To reduce the risk of infection (operations 2 and 3):
D) Bactroban ointment: Applied twice a day beginning 3 days prior to surgery x 7 days.
E) Hibiclens shower: Hibiclens soap applied to upper torso and abdomen – left on for 5 minutes, then rinsed. Applied once a day for 3 days prior to surgery.
F) Keflex: 250mg (antibiotic); one tablet 4x a day for 7 days, beginning with 2 doses the day of the operation.
To reduce postoperative nausea and vomiting (for each operation):
G) Emend: 40mg; one tablet by mouth the night before surgery
To reduce postoperative swelling and bruising (for each operation):
H) Arnica Forte (Arnica and Bromelain): two capsules daily x 7 days, beginning one day prior to surgery.
To help eliminate anesthesia from the system (for each operation):
I) Exchem: 10 drops in water or directly in the mouth twice daily, beginning the day before surgery and continuing for one week after surgery.
J) Lymphomyosot: 10 drops in water or directly in the mouth twice daily, beginning the day before surgery and continuing for one week after surgery.
To increase oxygen to the skin (operations 1 and 2):
K) Cutagenix: Applied to breast every 6 hours x 3 days. Skin care specialists use this topical cream after laser resurfacing to increase oxygen flow to the outer layers of skin. We decided in Angelina’s case to apply it to the mastectomy skin to give it an oxygen boost and to help ensure adequate blood flow to her skin postoperatively.
To minimize scarring (after operation 3):
L) BioCorneum: Rubbed into scars twice a day for 12 weeks – begin after the third operation once steri strips are removed.
Medications “as needed” for comfort:
Percocet: 1-2 tablets every 4-6 hours as needed for pain
Colace: 250mg twice a day
MiraLax: One tablespoon diluted in 8oz water once a day
Ativan: 1mg every 8 hours as needed for muscle spasm
Zofran: 8mg oral dissolving tablet placed on tongue every 6 hours as needed for nausea
LOCATION: Angelina chose to have her care, including her three operations, performed at the Pink Lotus Breast Center. Some people might think that a hospital is the only place to have a mastectomy. However, outpatient surgery centers provide an attractive, peaceful alternative when coupled with attentive nursing care at recovery facilities. You can learn more about our comprehensive and integrative breast center by exploring this website.
Stage 5. Recovering from the operations
On February 2, 2013, Angelina was in the operating room for the first operation, the nipple delay. Her partner was on hand to greet her as soon as she came around from the anesthetic, as he was during each of the operations.
After the operation, her skin was slightly bruised but soon returned to normal. Two days after her procedure, great news arrived: the tissue behind both nipples came back completely normal.
On February 16 she had the main surgery, which can last up to eight hours. The mastectomies went smoothly, with sentinel nodes identified but not removed. After the mastectomies, I assisted plastic surgeon, Dr. Jay Orringer, as we performed the first stage breast reconstruction by placing tissue expanders with allograft.
To a large extent, I believe recovery reflects expectation. Angelina expected to feel well, to be active. On Monday, the pathology returned and I called Angelina to confirm our biggest hope: all of the breast tissue was benign. On day four after her mastectomies, I was pleased to find her not only in good spirits with bountiful energy, but with two walls in her house covered with freshly assembled storyboards for the next project she is directing. All the while she spoke, six drains dangled from her chest, three on each side, fastened to an elastic belt around her waist.
The next day she had her first injection of saline into the expanders, thus beginning the process that would gradually prepare the tissues for the final stage of her operations, reconstruction. Four of the six drains were removed. Four days after that, on postoperative day nine, the last two drains were removed. A second saline fill occurred on March 4. Over the next four weeks she was hard at work.
The final operation occurred on April 27, 2013, ten weeks after the mastectomies: reconstruction of the breasts with implant, which went extremely well, bringing an end to her surgical journey.
Conclusion
Many women unfortunately do not know that BRCA gene mutations exist and could affect them. Breast and ovarian cancers take lives every day – knowledge and action can help prevent the premature loss of those who love us, and whom we deeply love in return.
Like Angelina, I urge women who feel they might have reason to be at risk for a BRCA gene mutation – perhaps because of a strong family history of cancer – to seek medical advice and to take control of their futures.