What is Menopause?
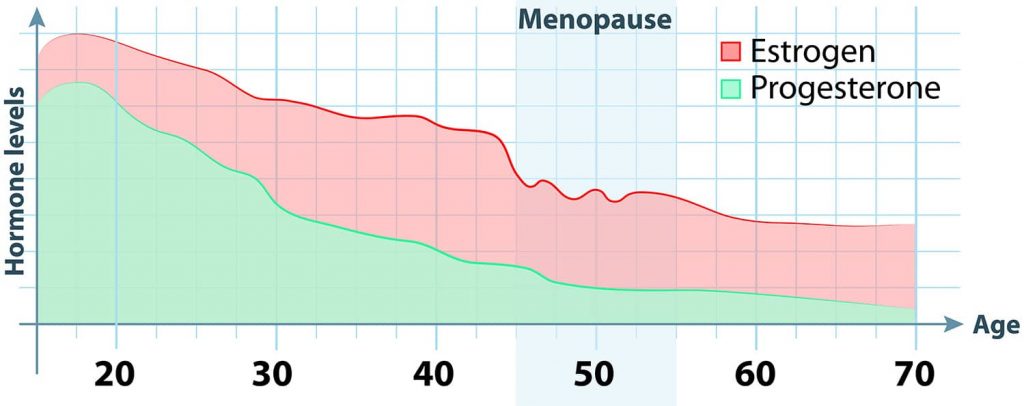
The on-paper, clinical definition of menopause is to be without a period for 12 months. At this time, your ovaries no longer make eggs and your estrogen and progesterone levels are plummeting, signaling the end of your reproductive years.
Common Symptoms
For the average woman, menopause is way more than just the end of her menstruation. It is the varied symptoms that affect her life before, during, and even after menopause. How many symptoms a woman experiences and to what degree, of course, varies. Some women breeze into menopause with their only symptom being the loss of their period, while others experience one, two, or many more symptoms from the list below:
- Hot Flashes / Night Sweats
- Insomnia
- Mood Changes
- Brain Fog
- Vaginal Dryness
- Lost or Diminished Libido
- Painful Intercourse
- Memory Loss
- Joint Discomfort
- Fatigue
- Nervousness
- Headaches
- Vertigo
- Palpitations
- Paresthesia (Tingling Skin)
- Formication (Crawling Skin)
- Urinary Urgency
- Increased Urinary Tract Infections
In what is called natural menopause, symptoms start during the transitional stage when a woman’s ovaries are making less and less estrogen and progesterone. This stage before menopause is called perimenopause and can last anywhere from a few months up to 10 years. Given that the average age range for natural menopause is mid-40s to mid-50s, it is possible to start experiencing perimenopausal symptoms as early as your 30s.
 We’ve been working hard on this. Add your e-mail address and we will tell you as soon as it launches.
We’ve been working hard on this. Add your e-mail address and we will tell you as soon as it launches.
Induced Menopause
For the majority of women who experience natural menopause, this process is gradual. For others, however, menopause happens literally overnight. This type of menopause is called induced and is a result of a medical procedure, such as a total hysterectomy with removal of both ovaries (called a bilateral salpingo-oophorectomy) or damage to the ovaries by drugs (e.g. chemotherapy) or radiation therapy, or from taking a medication that inhibits the effect of estrogen in your body, such as tamoxifen.
Surgically-induced menopause due to the removal of your ovaries is permanent and immediate. For women undergoing chemotherapy treatment, induced menopause can be somewhat more gradual and either temporary or permanent, depending if the ovaries can recover from chemotherapy’s likely cell damage. Age is a determining factor as well. Between 25%-50% of women in their 30s can expect a return of their periods, while 70-90% of women older than 40 will experience permanent menopause after chemotherapy.
This means that the age for induced menopause can occur at any time after puberty. It also means that a 25-year-old woman undergoing chemotherapy treatment can be put into immediate menopause, with the overnight drop in her hormones bringing on symptoms sudden and severe.
However the symptoms occur – naturally or induced, abrupt or gradual – the question always remains the same. How can you get and feel better?
Get discounted Tier 2 tickets while they last. Watch the Summit via on-demand video from anywhere or attend in person at the breathtaking oceanfront Terranea Resort in Southern California.
Hormone Replacement Therapy and Associated Risks
One of the first things women think of when contemplating how to address their menopausal symptoms is hormone replacement therapy (HRT). HRT is the use of hormones, either estrogen alone or estrogen in combination with progesterone, which is used to reduce menopausal symptoms, including hot flashes.
HRT can come in the form of a patch, pill, cream, gel, topical spray or a vaginal cream, gel, or ring. The problem with HRT is that it can come with many side effects, including diarrhea, acne, double vision, and brown/black patches, to name just a few. More importantly, as Dr. Kristi Funk explains in detail in her bestselling book, Breasts: The Owner’s Manual, there are also potentially serious risks involved with HRT, including breast cancer.
Why is that? In one word: Estrogen.
Estrogen can bind to cancer cell receptors changing the cells’ behavior for the worse. When the receptor and hormones are bound together, they attach to parts of the DNA inside your cell’s nucleus and tell your cells to keep dividing and dividing out of control, culminating in a cancerous tumor. Your cell could care less if the estrogen comes from your body or from the chemical inside the HRT. The process is the same. (Don’t worry, there are plenty of non-HRT options available to you, which we discuss later in this post.)
So what if you never had breast cancer and aren’t high risk? Unfortunately, HRT is still highly problematic.
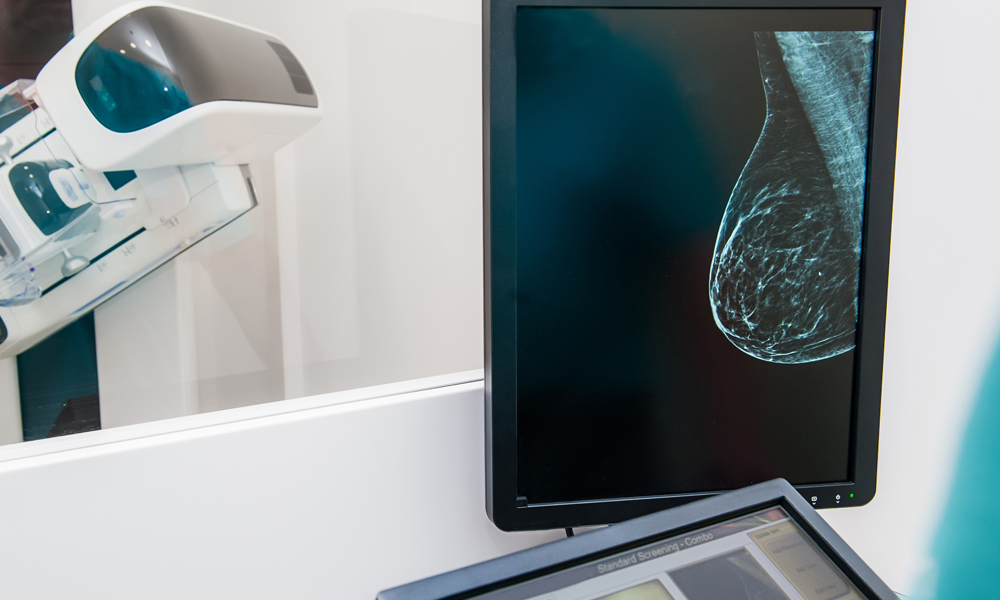
To start, one of the most common side effects of HRT is an increase in breast tissue density; 75% of HRT users see an increase. And having denser breasts immediately puts you into a higher risk of breast cancer, in part because tumors can hide behind the thick, white tissue. There are additional strikes against HRT, namely two large studies with shocking results.
Follow Power Up
Follow Power Up
The Women’s Health Initiative and the 1 Million Women UK Study
The Women’s Health Initiative was a long-term national study focused on strategies for preventing heart disease, breast and colorectal cancer, and osteoporotic fractures in postmenopausal women, which randomized 16,000 postmenopausal women to either an HRT with estrogen plus progesterone or a placebo.
This study was halted after just five years for ethical reasons because 26% percent more breast cancers had accrued in the HRT users, along with other serious health risks such as heart attacks, strokes, blood clots, and dementia.
In response to this study, in 2003, a staggering 33 million women immediately quit HRT and, with that, breast cancer rates plummeted almost 7%. In that same year, the UK published its observation of more than one million women in a different study: HRT was found to cause a 66% increase in breast cancer.
The Conclusion on HRT
Putting everything together, there’s no denying it: HRT energizes breast cancer, while quitting HRT reduces breast cancer. Does this mean hormones are off the table? Not necessarily. The conclusions above pertain to the use of HRT’s with estrogen plus progesterone. So what about estrogen-only HRT?
If you are specifically looking to reduce the symptoms of vaginal dryness and atrophy, topical vaginal estrogen can be very effective. Topical vaginal estrogen is different from HRT in that very little estrogen is absorbed into your bloodstream.
If you choose to use estrogen-only HRT, your cancer risk can increase or decrease depending on what age you start this type of HRT and for how long. Confusing, I know.
Specifically, women who take estrogen-only HRT for ten years yielded 23% less breast cancer. That’s good, right? Well, there’s a however – and a pretty big one at that. If the estrogen-only HRT use occurs within five years of menopause (when you would want it the most), there is a 57% increase in breast-cancer risk. The same increased risk is true if you take the estrogen-only HRT for more than 10 years.
To decide if hormones are for you, first and foremost, clearly understand your personal medical history and risks. If you decide to use estrogen-only HRT wait at least five years into menopause (so, six-years after you officially had your last period) and definitely discontinue using estrogen-only HRT when you near the 10-year use mark.
Bioidentical Hormones (BHRT)
While HRT contains hormones made in a lab (specifically from the urine of pregnant mares), bioidentical hormones are made from animal or plant sources, such as soybeans or yams. While this sounds less harmful than HRT, the problem is two-fold:
First, BHRT from compounding pharmacies are not regulated by the FDA for uniform dosing and purity. Instead, compounding pharmacies create personalized blends to meet individual needs. Secondly, we just don’t know if BHRT – whether from a compounding pharmacy or ones that are FDA-approved – are safe. To date there have been no large volume, high quality clinical trials (like The Women’s Health Initiative) to prove BHRT’s efficacy and safety. Until such a study, Dr. Kristi Funk’s advice – whether you use HRT or BHRT – is to use the lowest dose that controls your symptoms and for the shortest amount of time possible.
Without hormones, what are your remaining choices?
Natural & Non-HRT Treatment Options
Because the hormones in HRT are what instigate the growth of cancer, using a non-hormonal or non-estrogenic alternative is critical for an effective and safe alternative to ameliorating your menopausal symptoms.
Let’s look at your options, including cost, possible side effects and which symptoms you can expect to get relief from. Some lower-cost herbal products like Black Cohosh, Evening Primrose Oil and Ginseng provide relief for a specific set of symptoms, while other specialty botanical supplements like the bestselling Menopause Miracle offer clinically-proven comprehensive relief for a wide range of menopause and peri-menopuse symptoms, but at a higher cost. Your symptoms, budget, and the possible associated side affects, all play a role in which solution may be most suitable for you unique situation.[/vc_column_text]
You are Empowered
Some of the most important changes you can make to minimize your menopause symptoms are the same ones needed to reduce your risk of breast cancer and other diseases. And it’s something you can – and should – start now: Lead a healthy, active lifestyle combined with a reduction in environmental toxins.
Science supports this as well. Menopause studies show that switching from a sedentary lifestyle to one that includes some exercise results in both positive physical and emotional changes (see clinical study). Ramping up your exercise even further to include a cardiovascular workout can also help kick your hot flashes to the curb (see study abstract).
Eating right helps, as well – not just with your symptoms, but with reducing your risk of breast cancer and other diseases. A friend in your menopausal journey are plants with phytoestrogens (foods containing estrogenic qualities).
Foods with phytoestrogens, specifically isoflavones found naturally in whole foods such as tempeh, sprouted tofu, and edamame, can potentially minimize your menopause symptoms such as hot flashes. (Isoflavones isolated from soybeans, however, are not recommended due to their negative affect on estrogen-receptor-positive breast cancer.) Using soy milk in a smoothie is an easy way to get your phytoestrogens.
Need some ideas? Watch the video about the cancer kicking antioxidant smoothie Dr. Kristi Funk prepares each morning to start her day (it works great for breakfast, lunch, dinner or any time!)
Other ways to manage menopause symptoms are through focused breathing and gentle, flowing movement and stretches. Exercises such as Tai Chi, stretching, and Yoga combined with focused breathing can minimize menopause symptoms while increasing your overall quality of life. The wonderful thing about these low-stress exercises – and techniques like body-movement feedback where you are taught to voluntary control your muscle tension, heart rate, temperature, and brain activity – is that they can be done by people of any age. Start now and keep doing them way beyond your menopausal years.
Whether your menopause symptoms are minimal or are greatly affecting your life, always remember that there is no need to needlessly suffer. After all is said and done if you are still not feeling well – and especially if you are depressed – work with your health-care practitioner to find your path to empowerment and wellness.
You deserve it!